STIs | Sexually Transmitted Infections: Statistics, Diagnostics and Risks Minimizing

Content:
- What are STDs and STIs?
- STDs are actually more common among older generations!
- Statistics of STDs in Canada
- The list of STDs is constantly being reviewed
- Statistics of Chlamydia in Canada
- Statistics of Gonorrhoea in Canada
- Statistics of Syphilis in Canada
- Statistics of HIV in Canada
- Diagnostic Testing For Sexually Transmitted Infections
- STIs | Sexually transmitted infections: Minimize Your Risk
- Get vaccinated: bacterial and viral STIs
- Which vaccines for viral STIs exist
- Reduce the number of partners
- Always use condoms
- Learn to prioritize and say no
What are STDs and STIs?
Sexually transmitted infections (diseases) or STI (STD) are infections that can be transferred from one human organism to another through sexual intercourse. Some infections can also be transmitted from a pregnant woman to the fetus or through blood contact (contact through cuts on skin, blood transfusion, etc.). Unless they are treated properly, STI will develop freely in the body, and some of them may cause serious health issues.
STDs are actually more common among older generations!
Even though the medical science has been able to come up with cures for most sexually transmitted infections, they remain a rather common reason for visiting the doctor. Canada is no exception to the general rule, as STI have been on the rise there since the 1990s. One could assume that it would be the younger generation that suffers from sexually transmitted diseases most, but the statistics say otherwise. According to the most recent statistic data, people who are older than 39 have become almost as susceptible to sexually transmitted infections as the younger generations.
Statistics of STDs in Canada
 In Canada, the number of people who suffer from STI has been increasing since 1997. It is unclear to this day whether this increase is due to the improvement of the public healthcare system (more infections are diagnosed) or due to the factual rise in the numbers of infected people. Whichever reason it is, STI remain one of the major concerns of modern medicine. In 2008, more than two-thirds of almost 162,000 reported cases of notifiable diseases in Canada were caused by infections that are transmitted through sexual or blood contact, with chlamydia accounting for more than half of these cases. This tendency is no different from the ones observed in other developed countries of the world, particularly in the United States and Australia.
In Canada, the number of people who suffer from STI has been increasing since 1997. It is unclear to this day whether this increase is due to the improvement of the public healthcare system (more infections are diagnosed) or due to the factual rise in the numbers of infected people. Whichever reason it is, STI remain one of the major concerns of modern medicine. In 2008, more than two-thirds of almost 162,000 reported cases of notifiable diseases in Canada were caused by infections that are transmitted through sexual or blood contact, with chlamydia accounting for more than half of these cases. This tendency is no different from the ones observed in other developed countries of the world, particularly in the United States and Australia.
The Canadian Notifiable Disease Surveillance System (CNDSS) is responsible for most STI statistics available. It pursues the goal of collecting as much accurate information as possible. This is a rather complicated task, since for an infection case to be acknowledged by the CNDSS. It first has to be reported to a doctor by a patient. Many patients don’t experience any symptoms of STI or ignore them even if they do, so those cases go unnoticed by the healthcare system. Another source of possible statistical error is the fact that women tend to seek professional medical help more often than men. That could distort statistical data and make the CNDSS reach the conclusion that women are more prone to STI than men.
The list of STDs is constantly being reviewed
The list of notifiable diseases is constantly reviewed by healthcare professionals so that it is filled with as many entries as possible. That allows for more effective data processing and, as a result, more precise numbers concerning each of the infections. Some STIs have been subject to tracking since the beginning of the 1920s (gonorrhoea and syphilis, for instance), while others were only included in the list at the end of the 20th century (i.e. chlamydia). Herpes and papillomaviruses are still not on the list because they don’t pose an immediate threat to the patient’s health. It is known, however, that about 70% of all Canadians have contracted these infections at least once in their lives.
Statistics of Chlamydia in Canada
The infection known as chlamydia is more widespread than all other STDs in Canada, as it is about three times as common as gonorrhea and 50 times more common than syphilis. As a result, it is on the top of the list of sexually transmitted diseases in Canada. Unfortunately, according to various surveys, people hardly seem to know anything about this disease and, as a consequence, do not take necessary precautions to prevent infection.
This infection is caused by a bacteria called Chlamydia trachomatis, which acts as a secret weapon, often showing no symptoms. Partly due to this feature, chlamydia is able to spread with great speed. About 125 infected Canadians per 100,000 were reported in 1955, which was only the beginning of an upward trend. A half-century later, in 2010, the numbers have increased twofold, and there were more than 275 inhabitants of Canada diagnosed with chlamydia. Overall, the chlamydia-infected population of Canada increased from 1997 to 2010 by an impressive 143%.
More facts about Chlamydia: http://www.mycanadianpharmacyrx.com/can-chlamydia-bacteria-trigger-premature-ejaculation.html
In 2010, the number of infected women doubled compared to 1995, and reached almost 400 women per 100,000 Canadian residents. At the same time, in 2010, the number of infected men was close to the number of women reported in 1995. In a nutshell, the women-men ratio of chlamydia infection is 2:1. The highest number of patients suffering from chlamydia was recorded in 2010, when more than 2,000 per 100,000 young women aged from 20 to 24 reported chlamydia symptoms. Furthermore, 63% of 24-year-old people are estimated to have chlamydia, which makes 24 the most vulnerable age. Interestingly, women tend to be more sensitive to chlamydia, as around 70% of women experience no symptoms of the infection, compared to 90% of men who remain ignorant of having been infected by the bacteria.
This data was obtained by national agencies by observing both infected people and those who showed no visible symptoms of having contracted Chlamydia trachomatis. Overall, about 94,690 cases of chlamydia infection were reported in Canada in 2010. The provided statistics should be taken seriously, as it is highly important to be aware of the danger and know the ways of preventing it. Chlamydia can be treated with antibiotics, even though sometimes, when the patient hasn’t received timely treatment, there might be some severe side effects like pelvic inflammatory disease, fertility loss, and pneumonia for women and penile or testicular disorder for men. All of these complications can be prevented by careful use of protection for sexual intercourse.
Statistics of Gonorrhoea in Canada

Another infection that is currently being tracked by CNDSS is gonorrhea. It is also a very common STI in Canada, ranking second after chlamydia. It can have rather grave consequences for both man and fepatients. Women who do not get proper gonorrhea treatment can even become infertile, and in rare cases, gonorrhea can impact the blood stream. For females, the most “dangerous” age in terms of contracting gonorrhea is reported to be between 15 and 24 years, while for men it is estimated to be between 20 and 29. The fact that gonorrhea is becoming more and more resistant to the antibiotics that were traditionally used against it represents a major concern among medical practitioners.
In 1995, 20 Canadians out of every 100,000 reported gonorrhea. In the following two years, there was a slight decline, followed by a slow yet steady rise that began in 1997 and reached its peak in 2008, when the number of reported gonorrhea cases had grown almost twofold, reaching 38 people per 100,000 Canadians. Since that time, gonorrhea cases have become slightly less frequent.
Gonorrhea seems to be more common in the man population, with 22 and 38 reported cases per 100,000 people in 1995 and 2010, respectively. In women, these numbers amounted to 17 and 30, which is considerably less. In the period between 1997 and 2008, the difference was even greater, peaking in 2005 and 2006 at about 15 cases per 100,000. What is interesting, however, is the fact that the relative increase in the number of patients was higher in women.
Statistics of Syphilis in Canada
 Syphilis is an infection that is noticeably less common than chlamydia and gonorrhea, but its consequences can be just as bad, if not worse. Unless it is treated, syphilis can progress through 4 developmental stages: primary, secondary, early latent and late latent stages. While each of them has its own characteristics and presents its own threats to the normal function of the body, the most dangerous is the late latent stage. At that last phase, it can no longer be transmitted to other people, but it begins to destroy the host organism, causing disruptions in the function of the nervous system, heart, eyes, and skin, as well as other organs. It has also been proved that syphilis-infected people can be more vulnerable to human immunodeficiency virus.
Syphilis is an infection that is noticeably less common than chlamydia and gonorrhea, but its consequences can be just as bad, if not worse. Unless it is treated, syphilis can progress through 4 developmental stages: primary, secondary, early latent and late latent stages. While each of them has its own characteristics and presents its own threats to the normal function of the body, the most dangerous is the late latent stage. At that last phase, it can no longer be transmitted to other people, but it begins to destroy the host organism, causing disruptions in the function of the nervous system, heart, eyes, and skin, as well as other organs. It has also been proved that syphilis-infected people can be more vulnerable to human immunodeficiency virus.
Syphilis can be transferred not only through sexual intercourse, but also from mother to child. However, such cases are not very frequent in Canada. Only transmittable syphilis is subject to CNDSS tracking.
From 1995 until 2001, syphilis was diagnosed rather rarely (less than 0.001% of the whole population). However, after 2001, the numbers of syphilis-infected people started to rise drastically, and by 2009 they had increased fivefold. Until 2001, the difference between the numbers of infected men and females was negligible, but in the following years, there was a dramatic increase in the number of infected men. From 2004 till 2007, it fluctuated, then grew again and eventually reached 10 people out of 100,000 in 2010. Meanwhile, in the whole period between 1995 and 2010, the number of infected women barely changed at all. Overall, the population group that is the most susceptible to syphilis is represented by men aged between 30 and 39.
Statistics of HIV in Canada
Human immunodeficiency virus is probably one of the most destructive sexually transmitted diseases, as it affects and disarms the organism’s protection against various bacteria, which is known as immunity. It makes the human body open to all kind of dangerous and even life-threatening infections. HIV can be transmitted not only during unprotected sex, but also through blood, air, pregnancy, breastfeeding, or even by talking or shaking hands with an infected person.
Since 2008, the infection rate of HIV has been rather stable and showing neither peaks nor falls. Nevertheless, in 2014, national human immunodeficiency statistics showed some fairly disappointing figures. The overall number of Canadians infected with HIV had reached 75500 at the end of the year, which was a considerably bigger number compared to 2008 (the difference equaled 7%, or 6500 people). The prevalence rate was approximately 213 infected people per 100,000 inhabitants. Despite the rapid spread of the infection, the death rate was on the decline. Compared to the 1990s, when the number of HIV-infected people was much smaller, the death rate has decreased considerably due to the invention and implementation of effective treatment.
However, the diagnosis rate was not that promising, as the estimated number of Canadians living with undiagnosed human immunodeficiency virus was 16,000, which equaled more than one-fifth of the total number of infected people. This meant that, basically, one of five Canadians was living with human immunodeficiency virus without even realizing it. Consequently, these people did not receive special treatment and might have unwillingly infected others, posing a clear danger to society. What is more, according to 2014 reports, there were more than 26,000 lethal cases of undiagnosed human immunodeficiency virus.
There are certain groups of people who are at risk. 28% of those who experience heterosexual sexual intercourse are most likely to be unaware of being HIV-positive, while 20% of drug addicts and 18% of gay men could be exposed to HIV. More than a half of HIV-positive Canadians are gay or have claimed to have experienced a person-man sexual relationship at least once in their lives. Almost 14,000 people were infected through IDU (injection drugs). Over 31% of HIV-infected people living in Canada have had heterosexual intercourse, and 15% of them come from HIV-endemic countries. The number of women who are HIV-positive is estimated at approximately 17,000. Finally, only 610 people were not infected through intercourse or drug injections, which represents only 1% of all Canadians that have contracted human immunodeficiency virus.
Diagnostic Testing For Sexually Transmitted Infections
Sexually transmitted infections, or STIs, sometimes fail to be diagnosed for a long time, due to the fact that they do not cause any symptoms. Because of that, it is highly recommended that any sexually active person be screened for STI on a regular basis.
There are, however, some particularly vulnerable categories of people, which include:
- Pregnant women
- Sexually active young people (under the age of 25)
- People with HIV
- Men who have sex with men
There is usually no need to seek the consent of parents if an underage person wishes to be tested for STI, but it may be demanded by some medical institutions. In other institutions, a parent may be notified about test results even if no permission is required.
HIV/AIDS
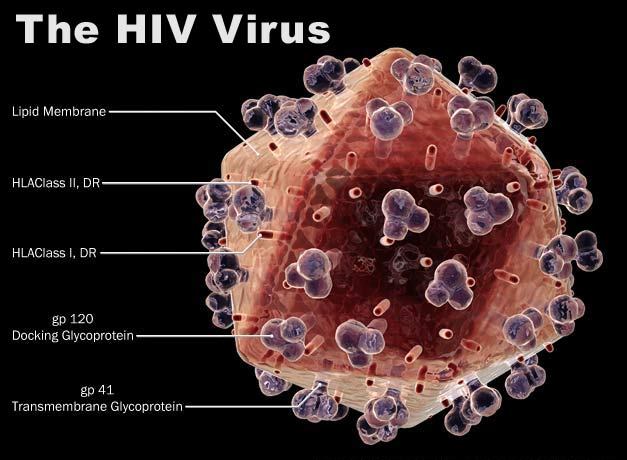
Both human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) can be detected through a series of identical observations and analysis, because AIDS is basically a consequence of HIV.
The fastest, and therefore not the most accurate way to check whether you are infected with HIV or AIDS or not is to take a rapid (conventional) HIV test. It helps detect specific antidotes in human body, the presence of which is indicative of the infection. The test can be conducted using samples of either blood or saliva. It takes anywhere from one to two weeks to obtain the results of the full test, while the results of a quicker but much less accurate test can be acquired in about 20 minutes.
Another way to diagnose HIV or AIDS is the ELISA test, which stands for an enzyme-linked immunosorbent assay. Similarly to the HIV test, it measures the amount of antidotes present in a blood sample. If any of the tests listed above provide an HIV-positive result, you will have to undergo some more serious laboratory observations, like the Western blot or an HIV nucleic acid test.
Chlamydia
Diagnosis of chlamydia begins with a physical examination, which includes a pelvic examination for patients. It helps examine woman’s genitals from the outside, which includes the examination of the womb, the cervix, the fallopian tubes that are responsible for carrying eggs to the uterus, the egg-producing organs, the bladder, and the rectum. It is highly recommended to take the pelvic exam at least once a year in order to detect infections and prevent them from spreading. This exam is also obligatory for pregnant women. If it so happens that you feel pain around your pelvis or lower back, you should take the pelvic examination immediately, as your symptoms could be caused by chlamydia or some other sexually transmitted diseases.
For males, the procedure is much simpler, as it involves taking a discharge sample from the man’s penis and testing it in the laboratory. Finally, both man and fepatients might be asked to bring a urine sample for a more thorough diagnosis. The results are usually presented within 1-2 days.
Gonorrhoea
The most common and scientifically approved way of diagnosing gonorrhoea is to take a NAAT, which stands for nucleic acid amplification test. It helps detect the DNA of Neisseria gonorrhoeae bacteria, which causes the disease. NAAT is also one of the most accurate tests for gonorrhoea.
Women are advised to take the nucleic acid amplification test in the following cases: blood coming from the vagina before or after a menstrual period or after having sex, painful feelings during sexual intercourse, and excessive excretions from the vagina. Unlike women, men might not have any visible symptoms, but it is necessary to take the NAAT if you notice that the colour of discharge from the penis has turned white, yellow or even green. Painful urination might also be a sign of gonorrhoea.
You can also take another test, which is called culture. It is performed on a sample of genital fluid by combining it with various substances that stimulate the growth of gonorrhoea germs.
Pelvic Inflammatory Disease
Pelvic inflammatory disease can be diagnosed in multiple ways. Sometimes it is simply identified by its symptoms, but should the doctor have doubts, he or she can perform an additional pelvic exam. During the exam, the doctor collects samples from the cervix and vagina. They are examined in a laboratory to identify the bacteria type that is causing the infection. Patients might also be asked to bring urine samples for the same purpose.
Some other tests might also be recommended to find out more about the infection. These include ultrasound testing of the feman reproductive organs, laparoscopy (a special instrument is inserted into the vagina so that the doctor can see it from the inside) and endometrial biopsy (a small sample of tissue is collected from the uterus and sent for laboratory analysis).
Genital Herpes
Genital herpes is rather difficult to diagnose, as it can show no symptoms at all, or produces symptoms that could easily be mistaken for those of some other infection. The first signs that you might be suffering from genital herpes prompting a visit to the doctor are sores on your genitals.
To make sure that the diagnosis is correct, the doctor should recommend additional tests. The PCR blood test is often used to determine if there are any herpes DNA residing in the patient’s blood. It is very accurate and detects the herpes virus even if the patient is not experiencing any symptoms. The doctor might also collect a sample of infected tissue from the sore and examine it under a microscope.
If the results of the two tests above seem to be false, the doctor might also recommend the antibodies test. A sample of tissue is collected from the sore once again and placed in a special solution that contains herpes virus antibodies and a special fluorescent dye. When the antibodies detect the virus in the sample, they gather around it and emit a glow that can be seen under a special microscope.
Syphilis
The first sign of syphilis can be diagnosed by the infected person themselves, as it is a little sore on their genitals, rectum, or in their mouth. It is called a chancre. However, people don’t usually notice it because it doesn’t cause any pain. Syphilis itself can go unnoticed for a rather long period of time because of showing no symptoms. Despite that, it is crucial to diagnose and start treating it as soon as possible, as it could be silently damaging the infected person’s internal organs.
The general symptoms of this stage are the following:
- Exhaustion
- Fever
- Weight and hair loss
- Pain in the joints
- Headaches
- Swollen and painful lymph glands
These symptoms are easy to confuse with a flu or some other common infection, so when they disappear, many infected people are unable to imagine that they will have to get treatment for syphilis.
However, if you’ve noticed some of these symptoms and you think that it might be syphilis, do not hesitate to seek professional medical help. It is possible to diagnose syphilis through blood and urine samples. A physical examination might also be conducted, and if there is a sore on your body, the doctor will collect samples from it and have them tested as well.
STIs | Sexually transmitted infections: Minimize Your Risk
Sexually transmitted infections (STIs) can have rather grave consequences, which is why it is so important to do your best to protect yourself from them. Sexual intercourse is an important part of many people’s lives, so it is crucial that at least one partner in a relationship is aware of the threats that STIs pose to the human body and is ready to share his/her knowledge.
First of all, learn more about sexually transmitted diseases. You don’t have to know everything about them, but try to become familiar with some basic information: what are the most common STI, their symptoms and consequences, how they are diagnosed and treated. There are also some other details that you might want to know. For example, who is more susceptible to a particular infection: men or women. All these bits of knowledge will help you on your way to protecting yourself from STIs.
Get vaccinated: bacterial and viral STIs
The next step is finding out more about STIs vaccines. There are two types of sexually transmitted infections: bacterial and viral. The former include gonorrhea, syphilis, and chlamydia. Such infections can be effectively treated with antibiotics, so it is not crucial to be vaccinated. However, the importance of such vaccines is underlined by the fact that sometimes, these diseases remain undiagnosed and, as a result, untreated. In such cases. the infection can silently cause damage to the body of the host person and be transmitted to other people. What’s more, medical practitioners are observing growing resistance of some STIs-causing bacteria to the antibiotics traditionally used against them.
Which vaccines for viral STIs exist
Viral sexually-transmitted infections include human papilloma virus, human immunodeficiency virus and hepatitis B. These diseases are harder to treat, so preventing them through vaccination is certainly a prudent “investment”. Unfortunately, vaccines for some viral infections are really hard to develop, so they are not widely available yet.
- Human Papilloma Viruses
HPV are astonishingly common: it is estimated that four women out of five will have contracted genital HPV by the time they are fifty. Genital HPV ionly one of many papilloma viruses, all of which have rather different symptoms and consequences. Some of them will go unnoticed, as the immune system is capable of neutralizing them without any need for medical intervention. However, some other HPV, if left untreated, will reside in the human body and cause certain types of cancer.
HPV vaccines are safe because they only contain samples of protein taken from some virus shells, not virus DNA. The vaccination is a series of three shots. The minimum age for HPV vaccination is nine for both boys and girls.
- Hepatitis B
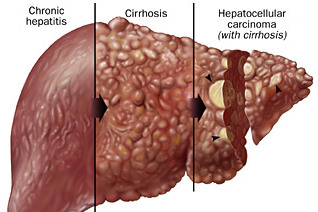
Hepatitis B is a disease that can be transmitted not only through sexual contact, but also syringe needles, razor blades, tooth brushes, open wounds and from mother to child. Most infected adults are able to make a full recovery from hepatitis B, while the minority (about 5%) will be chronically infected. Children are more likely to be permanently infected and they could suffer from liver dysfunction later in life.
The vaccine for Hepatitis B is strongly recommended for all children. It is done in three shots, starting shortly after birth. The next two doses are injected after rather long intervals of time. It is also recommended that people who live in places where the risk of contracting Hepatitis B is high are vaccinated as adults if they haven’t received the vaccine in their childhood.
The vaccines in development include vaccines for HIV and genital herpes. There are several vaccine candidates for both of these diseases, but none of them perform well enough to be released to the general public.
Reduce the number of partners
Even though you can protect yourself from some STI through vaccination, do not forget that there are STI with no vaccine available. The only foolproof way to avoid contracting them is having no sex at all. Since that is hardly reasonable, you should avoid having too many sexual partners. Studies have shown that people who have more than two sexual partners in one year face a significantly higher risk of contracting STI than those who have more stable relationships.
Being monogamous is also a good way of protecting yourself and your partner from STI. Honesty is really important in a mutually-monogamous relationship. Both you and your partner have to agree to be tested for STI and talk openly about the results. If both of you have no STI, being mutually-monogamous is the key to avoiding them.
It might also happen that one or both of you test positive for some STI. There is no need to panic, as most STI can be effectively treated. Once you are both sure that you are not infected, your long-term relationship will be your best protection from STI in the long run.
Always use condoms
Everyone knows that condoms are used to prevent unwanted pregnancy. However, if used correctly, they can also protect both partners from STI. The first thing you need to know is that if you intend to use condoms as a shield from STI, the condoms have to be latex. All other materials won’t do the job because they are more likely to break or slip. If you are allergic to latex, feman condoms will be the best alternative, as they are made of polyurethane. You’ll also have to make sure that the condom, whether man or female, covers as much skin as possible.
Learn to prioritize and say no
Some of your partners might refuse to use condoms. Sometimes, they might get forgotten in the heat of the moment. However, if you value your health (and your partner’s as well), you’ll have to be persistent. Try to talk to him/her and calmly explain why you insist on using condoms. Such a wish is no sign of mistrust, it is just a reasonable precaution to protect both partners from STI.
If he or she still refuses to do it, you can suggest that both of you get tested in a special clinic as a couple. That way, you can be relatively sure that unprotected sex is safe, as long as neither of you has sex with other people. Should your partner find this unnecessary, you’ll have to make an important decision: are you ready to put your health at stake to have sex with this person? Don’t be afraid to clarify your position if you don’t wish to risk it, because it is your health at stake and your right to choose.
Bear in mind that neither of these methods is capable of fully protecting you from STIs. The only way to achieve that is to never have sex at all. If you don’t find that possible, follow the above-mentioned rules and you will reduce the risk of contracting STIs to the bare minimum.
Information by My Canadian Pharmacy Research Group – www.mycanadianpharmacyrx.com

