Pulmonary Hypertension: What are the Causes, Symptoms, Diagnosis, and Treatment?
CONTENT
- Pulmonary hypertension – What is it?
- Why do pulmonary arteries become narrow?
- Are there symptoms of pulmonary hypertension?
- What can cause pulmonary hypertension
- How is pulmonary hypertension diagnosed?
- How is pulmonary hypertension treated?
- Medications
- Surgical therapy
- How should I manage my pulmonary hypertension?
- FAQs
Pulmonary hypertension – What is it?
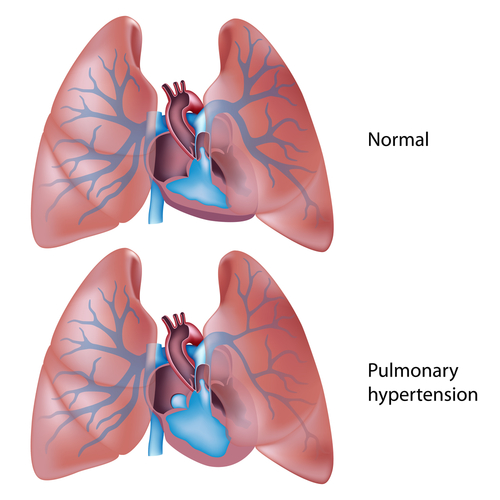
Pulmonary hypertention is a rarely-occurring lung decease that causes the arteries responsible for carrying blood to the lungs from the heart to shrink and narrow, which makes it more difficult for blood to flow through them. This causes another effect: the blood pressure in blood vessels (called “pulmonary arteries”) rises to abnormal levels. Consequently, the right ventricle of the heart is subjected to serious pressure and expands in size. However, it does not become stronger, it just gets overworked and over-enlarged, slowly losing the ability to pump blood through the arteries properly. This is a process that eventually develops into right heart failure.
Pulmonary hypertension can occur in any individual, despite positive factors of age, race or ethnic background. Nevertheless, it is a lot more common amongst young adults, and also occurs twice as rarely in men than in women.
Why do pulmonary arteries become narrow?
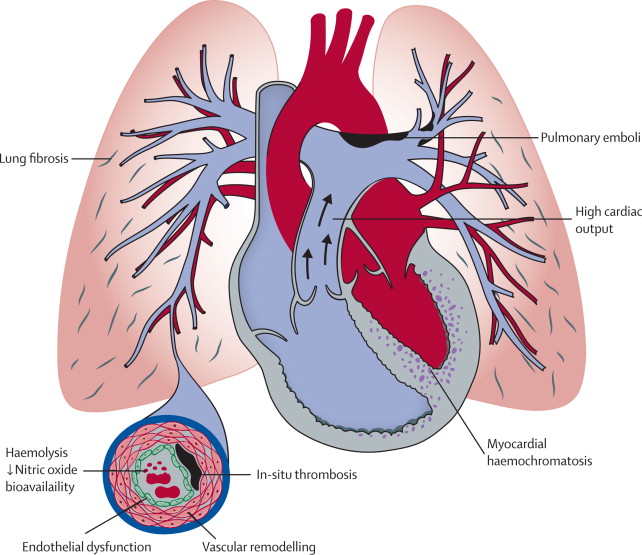
According to modern scientific knowledge, this process begins with an injury to the layer of cells that are the blood vessels of the lungs. The reasons why these injuries take place are unknown, but they substantially change the way these cells and the smooth muscle cells of the vessel walls interact, which makes the smooth muscles contract more than they should. Thusly, the vessels become too narrow.
Are there symptoms of pulmonary hypertension?
Yes, but not at the very first stage. Usually, symptoms occur only after the condition has progressed. At first, pulmonary hypertension presents itself through shortness of breath when you go through everyday activities such as going up the stairs. Fatigue, feeling dizzy, or fainting are also signs that may occur in the initial phase. If you notice swelling in the ankles, legs, or abdomen, if your skin or lips turn a bit bluish, if you feel pain in your chest – all of these symptoms are possible as the heart gets more and more strained. The severity of the symptoms can range significantly, starting with no symptoms at all, but at the later stages, any kind of physical activity can cause at least some of these symptoms.
In addition, symptoms can also include:
- racing pulse
- irregular heartbeat (strong, throbbing sensation, or palpitations)
- passing out or dizziness
- difficulty breathing at rest.
- shortness of breath during physical activity
And finally, any physical activity can become a serious challenge as the disease develops.
What can cause pulmonary hypertension?
The diet drug "fen-phen"
Even though the appetite suppressant “fen-phen” (made of dexfenfluramine and phentermine) has been taken off the market, the remaining users of fen-phen are 23 times more at risk of getting pulmonary hypertension, possibly over the course of several years.
Rheumatic disorders, liver diseases, lung conditions
Pulmonary hypertension can also occur as an outcome of other deceases and medical conditions, like rheumatic disorders such as scleroderma, systemic lupus erythematosus (lupus); chronic liver disease, liver cirrhosis; lung conditions, including emphysema, tumors, pulmonary fibrosis, and chronic obstructive pulmonary disease (COPD).
Some heart diseases
Certain heart diseases, including aortic left heart failure, valve disease, congenital heart disease, and mitral valve disease, can cause pulmonary hypertension.
Thromboembolic disease
The development of pulmonary hypertension can be caused by a blood clot forming in a large pulmonary artery.
Low-oxygen state
Living in a high altitude, sleep apnea, and obesity can also lead to pulmonary hypertension development.
Genetics
In a small number of cases, pulmonary hypertension is inherited. I you know that one or more of your family members has or had pulmonary hypertension, you should definitely take early precautions should symptoms occur.
It is important to remember that pulmonary hypertension is sometimes caused by other conditions, and in some cases, they remain unknown.
How is pulmonary hypertension diagnosed?
Since pulmonary hypertension can be caused by a big number of medical conditions, a full medical history analysis, a special physical exam, and complete description of all the symptoms are absolutely necessary for making a correct diagnosis and ruling out other deceases.
The physical exam will include:
- listening for abnormal sounds in the heart, like loud pulmonic valve sounds, systolic murmur of tricuspid regurgitation, and possibly a gallop caused by a ventricular failure;
- examination of the jugular vein, located in the neck for enlargement
- examination of the abdomen, ankles and legs, for fluid retention;
- examination of nail beds for a bluish shade;
- looking for signs of any other developing diseases that might cause pulmonary hypertension.
Other tests you should consider taking include:
- Blood tests
- Complete metabolic panel (CMP): A test for liver and kidney functions
- Autoantibody blood tests like ESR, ANA, and others: screening for collagen vascular diseases
- Thyroid-stimulating hormone (TSH): Thyroid problem screening
- HIV: Screening for human immunodeficiency virus
- Arterial blood gases (ABG): Defining the oxygen level in arterial blood.
- Complete blood count (CBC): Infection tests, tests for elevated hemoglobin, anemia
- B-type natriuretic peptide (BNP): A test for heart failure
- Doppler echocardiogram: Using sound waves to see the functioning process of the right ventricle and checking blood flow through the heart to measure the systolic pulmonary artery pressure.
- Chest X-ray: Reveals enlarged pulmonary arteries, as well as an enlarged right ventricle.
- 6-minute walk test: Defines one’s exercise tolerance level, and determines the level of oxygen in blood during exercise.
- Pulmonary function tests: Evaluates other possible lung conditions like idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease, among the rest.
- Overnight oximetry or Polysomnogram: A test for sleep apnea (which results in low levels of oxygen at night).
- Right heart catheterization: Examines various heart pressure issues (for instance, inside the pulmonary arteries, located on the left side of the heart), the rate at which it’s possible for the heart to pump blood, and reveals any leaks between the opposite sides of the heart.
- Ventilation perfusion scan: Checks the presence of blood clots along the pathways to the lungs.
- Pulmonary angiogram: Scans for blood clots blocking the pulmonary arteries.
- Chest CT scan: Scans for blood clots and other conditions that might be contributing to making pulmonary hypertension worse.

How is pulmonary hypertension treated?
A professional analysis and diagnosis of the condition is necessary before any treatment can begin.
Treatment will depend on a patient, and can vary according to different underlying causes, but usually includes:
- making lifestyle and dietary changes;
- taking medications;
- seeing your doctor regularly.
- undergoing surgery, if necessary;
Listed below are some medical and surgical treatment approaches.
Medications
There are various types of medications available for pulmonary hypertension treatment. Your choice, like one of those listed below, should depend on the severity of pulmonary hypertension, the likelihood of its progression, and the drug tolerance of the patient.
- Oxygen — to replace low oxygen levels in blood.
- Anticoagulants (aka “blood thinners”) like warfarin sodium (Coumadin) — to decrease blood clot formation, for blood to flow more easily through blood vessels. Important: when taking any anticoagulant medication, make a note to self to monitor any bleeding complications and regularly get lab work done to check the level of medication in your blood.
- Diuretics (or “water pills”) like spironolactone (Aldactone®), or furosemide (Lasix®)] — remove unnecessary fluids from the tissues and blood, which decreases swelling and allows for easier breathing.
- Potassium (like K-dur®) — replaces the essential nutrient potassium, that might be lost if increased urination takes place after taking diuretics.
- Inotropic agents (like digoxin) — increases the heart’s blood-pumping ability.
- Vasodilators [like nifedipine diltiazem (Cardizem®), or (Procardia®)] — decrease pulmonary blood pressure; potentially improve the blood-pumping abilities of the right side of the heart.
- Ambrisentan (Letairis®), bosentan (Tracleer®), macitentan (Opsumit) — allow the patient to block the activity of endothelin, a substance responsible for causing narrowed lung blood vessels. Taking these medications makes it essential to do monthly lab work for monitoring of liver function.
- Treprostinil sodium (Remodulin®, Tyvaso®), epoprostenol (Veletri, Flolan®), iloprost (Ventavis®) —widens pulmonary arteries and prevents blood clots from forming.
- Sildenafil (Revatio®), tadalafil (Adcirca®) — relaxes smooth pulmonary muscle cells, which allows the pulmonary arteries to dilate.
Surgical therapy
How should I manage my pulmonary hypertension?
Medication guidelines
- Know your medications and what they do. Keep a list.
- Take these medications at the same time each day. If you forget to take a dose, don’t take 2 doses at once to make up for the one you missed.
- Do not take any over-the-counter drugs if you haven’t consulted your pharmacist first. Some medicaments like decongestants (including Dimetapp, Benadryl, Sudafed and other drugs that contain pseudoephedrine or ephedrine), anti-inflammatory non-steroidal agents (like Advil, Indocin, and Motrin) can bring trouble to people with heart failure. Avoid any over-the-counter drugs with a statement on the label about risks for people with high blood pressure.
- Do not substitute or stop taking your medications if you haven’t discussed it with your doctor.
- Avoid herbal products – their effects are uncertain, when used with medications normally prescribed for pulmonary hypertension.
Dietary changes
- Eat food that is high in nutrients such as potassium (e.g. bananas, dried fruits, oranges), magnesium (e.g., tofu, peanuts, broccoli), vitamins.
- Limit your daily intake of calories, if needed to achieve your perfect body weight.
- Avoid products with a lot of saturated fats, sugar, cholesterol.
- Prefer high-fiber foods, such as whole grains, fruits, brans, vegetables.
- Reduce your daily sodium intake:
- Only buy foods with a low sodium level. Avoid seasoning salt and table salt.
- Avoid cured, smoked, canned, and salted meat products.
- Limit fast food and avoid prepared foods; they are usually rich in sodium.
- Monitor your daily fluid intake. Cut it down if you experience shortness of breath and/or if you notice any swelling.
Lifestyle changes
- Start monitoring your weight closely: check it at the same time each day and write it down on a calendar or in a diary. If you notice a fast gain in weight (2 pounds in 1 day or 5 pounds in 1 week), tell your doctor.
- Lose weight to reach your ideal weight (if needed)
- Go to health check-ups every year with your physician.
- Activity guidelines:
- Restrict pushing, lifting, or shoving to 20 pounds, as these activities increase pressure in your lungs and arteries.
- Walking is very important to keep the muscles strong and to increase circulation. More difficult forms of exercise, however, should not be done often, since your lungs might not be able to perform on the required level of productivity. Any sport or house activities that cause dizziness, shortness of breath, chest pain must be stopped immediately. See your doctor if any adverse symptoms occur.
- Do not chew or smoke tobacco.
- Reduce alcohol use or avoid it altogether.
- Avoid getting pregnant; use contraceptives.
- Keep in touch with your health care provider.
My Canadian Pharmacy Expert Group – www.mycanadianpharmacyrx.com
