Viagra Sensation: Does Sildenafil Aggravate PAH? My Canadian Pharmacy Study Report
A shocking scientific research has shaken the pharmaceutical society: a recent finding of research undertaken by Spanish cardiologist Dr. Javier Bermejo of Madrid University Gregorio Maranon General Hospital bears evidence that sildenafil contained in ED drug Viagra and PAH medicine Revatio can pose risks for patients with pulmonary arterial hypertension (PAH) and associated valvular heart disease. The irony of it will come through clearer as you read the contents of the article, but here is a brief recap of what it’s all about: the fact is that sildenafil is a product of a 1997 research aimed at finding a drug against… no, not impotence – PAH! Read on to learn the engaging details.
Historical facts: Viagra development
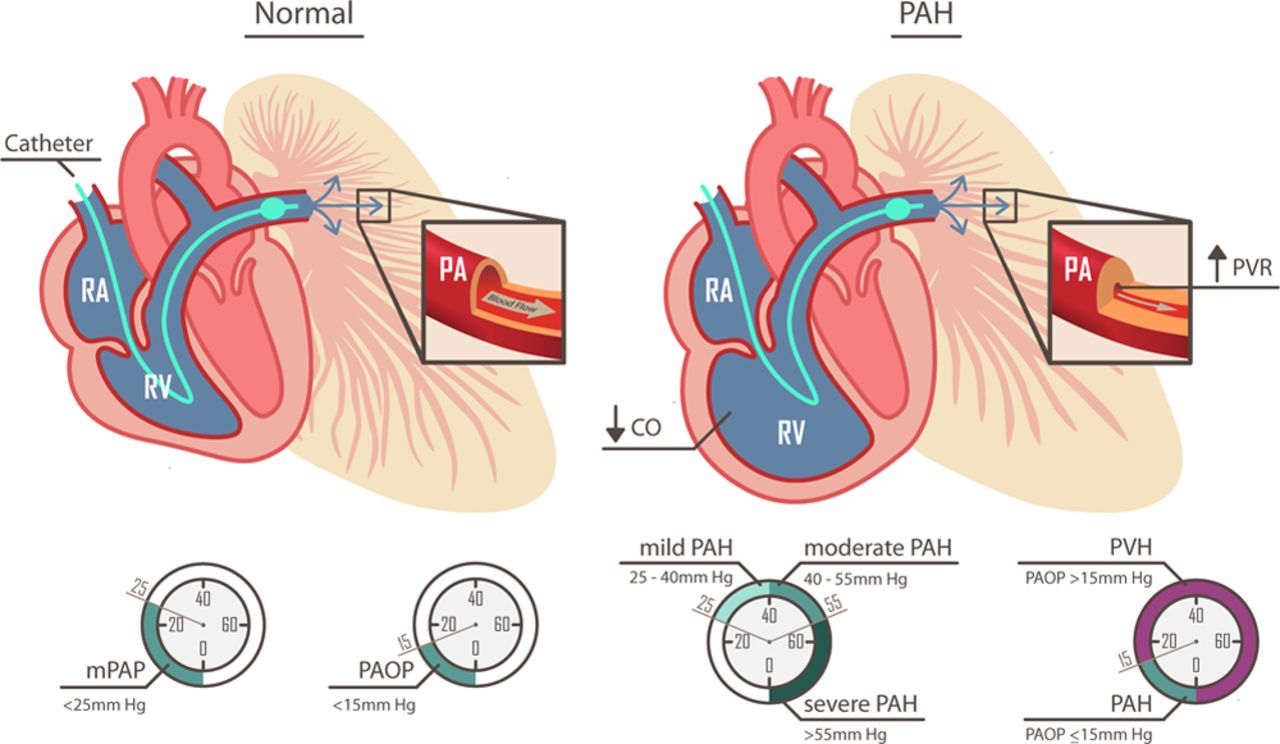
Sildenafil (the active component of Viagra, all generic Viagra types and Revatio) was invented as a result of a research whose objective was to find a drug for PAH. Pulmonary arterial hypertension is a pathological condition in which the blood pressure within the pulmonary arteries, and the right heart cavities, is elevated.
If you find this intersing, check out our Generic Viagra page for major informativity on the subject: mycanadianpharmacyrx.com/generic-viagra
The developing company had had a breakthrough success with the research in 1997: but during the trial phase, a side effect was discovered that changed it all: sildenafil was reported to have enabled men with erectile dysfunction (ED) and compromised sexual ability to recover erectile function for several hours. That was when the original purpose of sildenafil, that of PAH treatment, was moved into the background, outshined by the newly discovered feature that changed the way the game was played in ED treatment forever. Viagra became the first oral drug for ED therapy. Nowadays, the universally acclaimed sildenafil marketed as Viagra acts as a vasodilator and blocks the enzyme responsible for the disease. Its use against pulmonary hypertension (PAH) of children and teens divides scientists from the middle world.

But sildenafil’s original purpose was not at all forgotten and put to rest: until that day, the generic component is marketed under the name of Revatio and used in PAH patients. And here is where the sensational new research findings chip in.
This is how Viagra can cause heart risks in PAH patients
In his placebo-controlled study, Dr. Bermejo discovered that during 6 months of sildenafil therapy, patients suffering from valvular heart disease displayed worsening of symptoms of PAH linked to their cardiac condition. In this connection, the scientist suggests issuing a peer review and an official warning against the use of sildenafil as part of residual PAH treatment in individuals affected by valvular heart disease. Canadian Pharmacy reminds you that this claim still needs to be officially supported, but this is still pending and unclear. For now, read more evidence from the world of science supporting the results arrived at by the Spanish cardiologists.
New Scientist’s magazine alternates favorable and contrite opinions. Contracts denounce the lack of clinical trials that have verified the effects of the blue pill on children. To succumb to the use of Viagra, on the other hand, the encouraging results of some of the most prestigious experiences.
Learn more about Viagra effects in heart valve disease: Viagra May Harm Patients with a Heart Valve Issue
Many doctors who use Viagra to treat these children hope to start their studies even on the very young, and in the meantime administer the drug with the consent of the parents and the hospital structure. And it seems more effective than other drugs available. But there remains the problem of lack of experimentation. It is a question of many medicines given to children, although it is true that 90% of those used on infants and half of those prescribed for children are only recorded for adult use.
‘The problem is that pharmaceutical companies do not have to invest resources in pediatric medicine, because they are much more adults than children,’ commented Richard Nicholson, editor of the Bulletin of Medical Ethics. At present, the European Union is discussing a directive that would extend the patent for companies that decide to test children over six months.
To deepen your knowledge on the subject, My Canadian Pharmacy recommends proceeding to the paragraphs that follow.
What is pulmonary arterial hypertension?
Very often, this severe condition is related to a deterioration of the wall constituting the pulmonary arteries (or their branching): as a result of this alteration, the same arteries narrow down and the blood flow inside them is reduced. The main symptoms of pulmonary hypertension include dyspnoea, chest pain, fainting and tachycardia. To diagnose this condition properly, several diagnostic examinations are needed, which are also needed to trace cause triggers. Therapy can be pharmacological or, if the medications have poor results, surgical.
Before describing pulmonary hypertension, it is useful to rethink some of the core characteristics of the heart. The heart is divided into two halves, right and left. The right heart is composed of the right atrium and the right ventricle below. The left heart is composed of the left atrium and the left ventricle below. Each atrium is connected to the underlying ventricle by means of a valve. The right atrium receives non-oxygenated blood through the vein veins.
The right ventricle pumps blood into the lung arteries, leading it to the lungs. In the lungs, blood fills with oxygen. The left atrium receives oxygenated blood, returning from the lungs, through the pulmonary veins. The left ventricle pumps oxygenated blood into the organs and tissues of the human body through the aorta. Each ventricle communicates with its efferent vessel by means of a valve. Therefore, the heart valves are four in all.
The right heart cavities (including the vessels that come to you and leave you) are indicated by the blue arrows, while the left cavities (also in this case, including vessels) are highlighted with the red arrows.
Pulmonary hypertension is a serious pathological condition, characterized by prolonged elevation of blood pressure within the pulmonary arteries (or one of their branches) and inside the right cavities of the heart. People with pulmonary hypertension have difficulty in enduring mild physical efforts and are particularly predisposed to suffering from heart failure (or heart failure).
In most cases, pulmonary hypertension is established when the walls of the pulmonary arteries undergo an alteration, which is why they are narrowed or completely suppressed. This has two consequences: on the one hand increases the resistance that the blood encounters going from the heart to the lungs and on the other is obstructed the pumping action of the right ventricle.
In other words, at the origin of pulmonary hypertension there is almost always a vasoconstriction of the arteries that lead the blood from the heart to the lungs; such vasoconstriction reduces direct blood flow to the lungs and prevents the right ventricle from functioning normally.
Pulmonary arterial hypertension. It is further subdivided into the following subcategories: idiopathic pulmonary hypertension, hereditary pulmonary hypertension, lung-induced pulmonary hypertension or toxic substances, persistent pulmonary hypertension of the infant; pulmonary hypertension associated with other morbid states, including portal hypertension, HIV infection, connective tissue disease, and so on.
Pulmonary hypertension due to left heart dysfunction. The major dysfunctions affect the left ventricle and mitral valve and aortic valve.
Pulmonary hypertension due to pulmonary and hypoxic dysfunction. They are responsible for this type of pulmonary hypertension in the following morbid states or situations: obstructive chronic bronchopneumopathy (COPD), pulmonary interstitiopathy, sleep apnea syndrome, high altitude (above 2400-2500 meters), alveolar hypoventilation.
Pulmonary hypertension linked to chronic thromboembolism. Thromboembolism is a disease characterized by the tendency to the formation of blood clots attached to the wall of blood vessels (thrombi), which can detach itself and enter the bloodstream (embolisms).
Pulmonary hypertension due to other causes. They are responsible for this form of pulmonary hypertension in various diseases including: myeloproliferative disorders, sarcoidosis, neurofibromatosis, vasculitis, xystiocystosis x, gaucher disease, thyroid disorders, chronic renal failure, and compressive tumor masses.
Group I
Group I pulmonary hypertension is accumulated by causing vasoconstriction of blood vessels from the right ventricle to the lungs. Idiopathic pulmonary hypertension. In medicine, a disease is idiopathic when it occurs without an identifiable pattern. Idiopathic pulmonary hypertension is very rare (N.B: annual incidence is 2 cases per million people) and affects women predominantly.
Hereditary pulmonary hypertension. In some subjects, pulmonary hypertension is caused by a genetic mutation transmitted by parents. In these cases, the disease is considered to be a hereditary illness in all respects. Pulmonary hypertension induced by drugs and toxic substances. Some substances that may lead to pulmonary hypertension are fenfluramine and amphetamines.
Infant persistent pulmonary hypertension. According to statistical research, about 2 babies every 1,000 suffer from pulmonary hypertension. The latter is usually associated with morbid conditions or unhealthy health conditions such as: Septicemia, Hypoglycaemia, Severe Pulmonary Hypoplasia, Concomitant Concomitant Meconium, Pulmonary Hypertension associated with Other Morbid Conditions.
Some of the major morbid states that can be associated with pulmonary hypertension are:
- Connective tissue disorders such as scleroderma, systemic lupus erythematosus or rheumatoid arthritis. According to some statistical research, pulmonary hypertension is found in 21% of cases of rheumatoid arthritis and in 4-14% of cases of systemic lupus erythematosus (N.B: for scleroderma, the data is unclear).
- Congenital malformations of the heart.
- Portal hypertension. It is a pathological condition for which the pressure, within the liver vein, rises beyond the normal. Pulmonary hypertension occurs in 2-5% of people with portal hypertension.
- HIV infections.
- Thyroid gland disorders.
- Chronic hemolytic anemia (N.B: among variants of this type of disease there is also sickle cell anemia).
- Veno-occlusive lung disease.
- Pulmonary capillary emangiomatosis.
Group II
Pulmonary hypertension due to left heart dysfunction is a particular case. It is the only one that does not occur for the vasoconstriction of the pulmonary arteries, but for a problem with one of the supporting structures of the left heart (atrium, ventricle, mitral valve or aortic valve). About 60% of people with left ventricular dysfunction and about 2/3 of those with severe aortic valve defect also suffer from pulmonary hypertension.
Group III
In Group 3 pulmonary hypertension, vasoconstriction and other alterations in the pulmonary arteries are due to a reduction in oxygen levels in the blood (hypoxia). This reduction is often the result of an illness that affects breathing (such as COPD or sleep apnea syndrome).
Group IV
In pulmonary hypertension caused by the presence of blood clots (thrombi or emboli), the narrowing of the vascular wall occurs because the clots release substances that specifically cause vasoconstriction. The presence of an embolism at the level of the pulmonary arteries is a condition known as pulmonary embolism. Two people in 100 with pulmonary embolism also suffer from pulmonary hypertension.
Group V
Vasoconstriction of pulmonary arteries appears as a result of a still unclear pathogenetic mechanism. However, potential triggers are quite well known. At initial stages, pulmonary hypertension is often asymptomatic (i.e. lacking obvious signs and symptoms). With the worsening of vasoconstriction to pulmonary arteries, however, the first pathological manifestations appear. The main symptoms of pulmonary hypertension are: discomfort (or short breath), whether under stress (stress disorder) or at rest (dyspnoea at rest), dizziness , fainting and syncope, pain or chest pressure, edema in the legs, hips and, sometimes, even in the abdomen (ascites), kinesis , increased heart rate (tachycardia or palpitation), feeling of general fatigue
The occurrence of an unusual dyspnea during a minimal effort must induce the victim to contact your doctor immediately, for a closer look at the situation. In addition, symptoms and signs such as chest pain, edema in various parts of the body and cyanosis should be considered deserving of deepening.
In the long run, the condition of pulmonary hypertension may lead to the following complications:
- Pulmonary heart disease. It is a very serious cardiac disease, characterized, first, by an enlargement of the right ventricular cavity and, subsequently, by a thickening of the muscular wall constituting the right ventricle (right ventricular hypertrophy). These alterations are the adaptive response to shrinking lung arteries and the difficulties encountered by the blood crossing them.
- Tendency to the formation of clots inside the blood vessels that lead the blood into the lungs. Thromboses that cause the most severe effects are those affecting the smaller branches of the pulmonary arteries, as they easily encase such vessels.
- As the condition of pulmonary hypertension becomes worse, tachycardia may complicate with arrhythmias (i.e., heart rhythm alterations), even mortal ones.
- Bleeding in the lungs. The characteristic sign is hemoptysis, that is, blood coughing.
- Insufficienza cardiaca (o scompenso cardiaco). È la condizione patologica per cui il cuore non riesce a pompare efficacemente sangue verso tutti i distretti del corpo. Tra i sintomi classici, si ricordano la grave dispnea anche a riposo e il senso di stanchezza persistente.
- Pulmonary hypertension is difficult to diagnose because, even when symptomatic, it is very similar to symptoms and signs to other heart and lung pathologies.
Therefore, in order to be able to highlight the presence, the physician is required to submit the patient to various examinations and diagnostic tests.
Usually, after a thorough exam, there will follow blood tests, chest x-ray, echocardiogram, right heart catheterization, spirometry, analysis of pulmonary perfusion, CTA (Computed tomography angiography), nuclear magnetic resonance and pulmonary biopsy. The considerable number of diagnostic examinations is due to the fact that the physician, in addition to wanting to diagnose pulmonary hypertension, needs to determine the precise causes of the latter. In fact, once you find the cause of the disease, it is easier to plan proper treatment.
First, during the target examination, the doctor visits the patient and asks him to describe the symptoms. After that, he goes to the analysis of clinical history (current state of health, past illnesses etc.) and lifestyle habits (he wants to know, for example, whether the patient is a smoker, if he drinks alcohol, etc.).
Blood tests
Obtained by a simple withdrawal, the patient’s blood sample may have values associated with pulmonary hypertension because they are dependent on other associated morbid conditions (such as, for example, systemic lupus erythematosus). However, it is important to remember that blood tests are a little specific diagnostic method and require further confirmations.
Chest X-ray
The RX-chest provides a fairly clear image of the heart, lung arteries, lungs and any abnormalities. However, it has been noted that a significant proportion of patients with pulmonary hypertension (about 1/3) are completely normal for this test.
Echocardiogram
The Doppler echocardiogram is an ultrasound examination that shows in detail the appearance of the heart, its possible abnormalities and the blood flow dynamics through atria, ventricles and cardiac valves. It allows identification of valve defects, difficulty pumping the heart, and myocardial malformations (including cardiac cavities and wall thickening). Echocardiogram is a simple and non-invasive examination, which involves the use of an ultrasonic probe (transducer) resting on the chest of the patient.
Doppler echocardiogram variant
Sometimes, to get more specific information about the heart, doctors use the transesophageal echocardiogram. Its greater specificity is priced: in fact, the examination is invasive, as it involves inserting the transducer in the patient’s esophagus.
Right heart catheterization
Right heart catheterization is a delicate and somewhat invasive procedure, requiring the use of a particular catheter. This catheter, once inserted into an important vein of the body and brought to the right ventricle and pulmonary arteries, allows to measure blood pressure within the latter. In the case of pulmonary hypertension, average pulmonary arterial pressure in the rest is greater than 25 mmHg. Cardiac catheterization is performed in a specialized hospital department and involves local anesthesia.
Spirometry
Fast, practical and painless, spirometry records the inspiratory and exhalative capability of the lungs and the pervivability (i.e., the opening) of the airways passing through them. It is necessary to establish the functionality of the lungs.
Analysis of pulmonary perfusion
The exam studies the way the blood spreads into the blood vessels that reach the lungs. During the analysis, the physician inject a radioactive substance in a patient’s vein, visible with a suitable instrument. In subjects with pulmonary hypertension, highlights where the pulmonary arteries or their ramifications narrow down. The main disadvantage of pulmonary perfusion analysis is the use of radioactive materials. Caution: Patient perfusion analysis is combined with pulmonary ventilation (pulmonary scintigraphy) analysis (or V / Q scan or ventillus-perfusion scintigraphy).
CTA and nuclear magnetic resonance imaging
CTA (Computerized Axial Tomography) and Nuclear Magnetic Resonance (RMN) are two diagnostic imaging tests that, in the case of pulmonary hypertension, allow to highlight changes in lung arteries or their ramifications. CTA, unlike RMN, is an invasive examination, as it exposes the patient to a minimum dose of ionizing radiation. Pulmonary biopsy consists in taking and analyzing a small sample of pulmonary tissue coming from the patient. The withdrawal can be done by bronchoscopy, bronchoalveolar wash or surgical intervention.
Viagra’s active components sildenafil in PAH treatment – and other therapies
Establishing the correct therapy for pulmonary hypertension may sometimes be somewhat complicated. Treatment, in fact, varies from patient to patient, depending on triggering causes and other pathological conditions accompanying pulmonary hypertension (causal therapy). The following are the classes of medicines most commonly used in the treatment of pulmonary hypertension, and some examples of pharmacological specialties; it is up to the physician to choose the active ingredient and the most suitable posology for the patient, depending on the severity of the illness, the health of the patient and his / her response to the treatment.
First-line drugs for the treatment of pulmonary hypertension:
Generally, there is a combination of different drugs; the choice of the most appropriate association with the case occurs after some tests: medicines that, after such tests are more effective, are permanently prescribed.
However, it is important to remember that even the most appropriate pharmacological therapy does not completely cure pulmonary hypertension, but it only merely improves the associated symptoms. If any pharmacological treatment is to be ineffective, surgery should be considered. Before starting to analyze the possible drugs and treatments to relieve symptoms of pulmonary hypertension, we report schematically the mechanism that triggers the disorder, which will help to better understand the choice of therapeutic strategies.
Shrinking lung arteries → fatigue blood flowing in the lungs → pressure → right ventricle is forced to overdrive to pump the blood into the lungs → ventricle enlargement → heart weakening and heart failure.
Although no fully resolved cure for pulmonary hypertension has been identified, current therapeutic options are aimed at relieving symptoms, improving the patient’s quality of life and, above all, blocking or otherwise curbing the inexorable progression of the disease. It is imperative to intervene on factors that predispose or accentuate pulmonary hypertension, such as (in particular) apnea, pulmonary diseases and heart valve disorders.
The doctor will choose which drug is most suitable for the patient, depending on the cause (i.e., hypothesisable or confirmed, when discernible) and obvious symptoms; some assisted people need blood thinners to reduce the risk of clotting in lower limb veins or lung arteries. In many patients with pulmonary hypertension, low levels of oxygen in the blood are observed: in these cases, appropriate therapy (oxygen supplementation) is required. Patients affected by pulmonary hypertension should quit smoking, avoid going to high altitude locations, refraining from heavy physical exercise and lifting, and undergo annual influenza and pneumococcal vaccine. In cases of severity, heart, lung or both are thought to be transplanted.
Parallel therapies for the control of pulmonary hypertension symptoms

Some specialists also recommend taking standard medicines used in hypertension therapy; particularly indicated appear to be the calcium channel blockers (or calcium antagonists) and diuretics.
Anticoagulant therapy to prevent the complications of pulmonary hypertension. Isosorbide dinitrate (e.g. Carvasin, Dinike, Nitrosorbide): the drug is a nitrate, also used for the treatment of angina pectoris; is used as a second choice for the treatment of pulmonary hypertension symptoms. Start therapy with a dose of 40 mg every 8 to 12 hours. Continue with a maintenance dose at 40-80 mg every 8 to 12 hours.
Epoprostenol (e.g. Flolan, Epoprostenol PHT): it favors vasodilatation and inhibits platelet aggregation. For this reason, the drug is used in therapy to control the symptoms of pulmonary hypertension. Initiate therapy with a dose of 2 ng / kg / min; gradually increase the dose with increments of 2 ng / kg every 15 minutes. Do not exceed 8.6 ng / kg / min. consult your doctor for more information.
Scientists are addressing their research into the treatment of pulmonary hypertension to experiment with new drugs such as serotonin antagonists, soluble cyclanic guanilate stimulants, tyrosine kinase inhibitors and vasoactive intestinal peptide. We will have to wait a few more years before finding the truly miraculous – and therefore totally resolved – drug for pulmonary hypertension.
The surgical operations that can be used in case of pulmonary hypertension are:
Atrial septostomy. It is an ‘open heart surgery’, during which the practicing physician practices a small hole in the structure that separates the right atrium from the left atrium (interatrial septum). This should reduce blood pressure within the right heart and inside the vessels leaving it. Possible complications: after its execution, the patient may suffer from arrhythmias.
Heart transplant, lung or both. They are very delicate surgical interventions, during which they replace the malfunctioning organs with other healthy, coming from compatible dead donors. Possible complications: The patient who has undergone organ transplantation may reject the same organ following an abnormal immune reaction (transplant rejection). In addition, high intake of immunosuppressants (which are used to prevent rejection) is predisposed to infections.
- If you are suffering from pulmonary hypertension, it is good practice to comply with certain rules, including:
- Stay at rest when you feel the need.
- Practice physical activity regularly. Obviously, such physical activity must be commensurate with the state of health, as exaggerated efforts may be fatal.
- Do not smoke.
- If you are a woman, avoid getting pregnant, because pregnancy may worsen the situation. In addition, the life of the fetus is in danger.
- Avoid traveling or living at high altitudes.
- Avoid all situations that could greatly reduce blood pressure (hypotension), such as too hot baths or saunas. Excessive drop in blood pressure can lead to fainting and even death.
- Adopt a healthy diet and possibly low salt (hyposodic diet).
- Pulmonary hypertension significantly affects the quality of life of people affected. Its establishment, in fact, prevents many activities that characterize a normal existence.
The prognosis depends heavily on the time when the diagnosis is taking place and when the treatments begin: in fact, the more early the pulmonary hypertension is highlighted and cured, the greater the survival rate is five years after the diagnosis.
Read also interesting information about the use of Viagra:


